Shoulder injuries are some of the most common results of trauma and are frequently the subject of litigated personal injury claims. But when it comes to the “shoulder injuries,” one size does not fit all. A shoulder injury is a generic term that can be used to describe damage to any number of the bones, joints, ligaments, and tendons in the upper extremities. These injuries will vary in degree of severity and painfulness. Additionally, treatment for such injuries can vary from taking anti-inflammatory medication and resting, all the way to open surgical procedures utilizing hardware such as anchors, screws, and plates. Here we discuss some of the most commonly seen shoulder injuries that can occur as a result of an accident or trauma.
I. FRACTURES
The clavicle, or collar bone, is the bone that connects the sternum/breastplate to the shoulder. Traumatic clavicle fractures are common, given the relatively small size of the bone. Fractures of the clavicle most often in the middle of the bone (mid-shaft) and, less often, close to the acromion or breastplate.
Symptoms of a clavicle fracture include pain and discomfort as well as the swelling at the fracture site. Open fractures of the clavicle (where the bones pierces through the skin) are rare, however displaced fractures are not uncommon. Clavicle fractures – like most injuries to a bony structure as opposed to a soft structure such as a ligament, tendon, or muscle – are diagnosed with an x-ray.
Clavicle fractures are mostly commonly caused by a fall either directly on the shoulder or onto an outstretched hand. Direct trauma to the clavicle itself can also cause a fracture, though given the force required for a direct-impact fracture, these are less commonly seen.
Treatment for a clavicle fracture is often non-operative. Evan displaced fractures can be treated conservatively without surgery. The affected arm will be immobilized in a splint for, depending on the severity of the fracture and healing, anywhere from 4 to 8 weeks. In severe cases, surgery may be required, which entails plating and screws to join the two fractures pieces of the bone together.
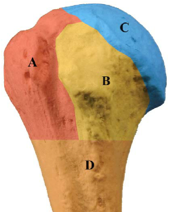
The humerus is the long bone that runs from the shoulder area to the elbow. The proximal aspect of the humerus is nearest to the shoulder and is comprised of the (A) greater tuberosity, (B) less tuberosity, (C) articular or head, and (D) shaft. Fractures of the humerus are often described based upon how many of the above parts of the humerus are damaged, e.g., a one-, two-, three-, or four-part fracture.
Like clavicle fractures, the most common cause of a humerus fracture is due to a fall on the shoulder or on an extended arm.
Although humeral fractures are treated non-operatively, there is a greater incidence of surgical cases resulting from a humeral fractures when compared to clavicle fractures. The extent of the surgery, as with all surgeries, depends upon the extent of the fracture. Surgery can include locking pates and screws and/or intramedullary nails. A shoulder replacement can also be performed on a total or partial basis as treatment for a humeral fracture. Replacements, called arthroplasties, are most often considered for older adults and those with bone density loss.
An avulsion fracture occurs when a flake or chunk of bone attached to a tendon or ligament gets pulled away from the main part of the bone. When significant pressure is exerted on the ligament/tendon due to trauma, the tension can cause the point where the ligament/tendon attaches to the bone to pull away a part of the bone.
Avulsion fractures can occur in most areas where a ligament or tendon attaches to a bone. An example of an avulsion fracture of the shoulder occurs within the greater tuberosity and is depicted below. This type of shoulder fracture happens when the supraspinatus and/or infraspinatus muscles are overloaded, often due to a direct trauma with dislocation.
The extent of the fracture can vary. Avulsion fractures are more often non-displaced than displaced, making them very difficult to identify on x-rays. The size of the bone fragment can vary from a small chip to a larger chunk of bone. If the fracture is non-displaced, it will often heal without the need for surgical intervention. If, however, the fracture is displaced, surgery using anchors, screws, and possibly plates may be necessary to reattach the bone fragment to the larger bony structure.
II. SHOULDER TEARS
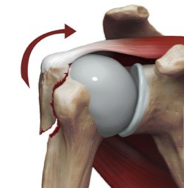
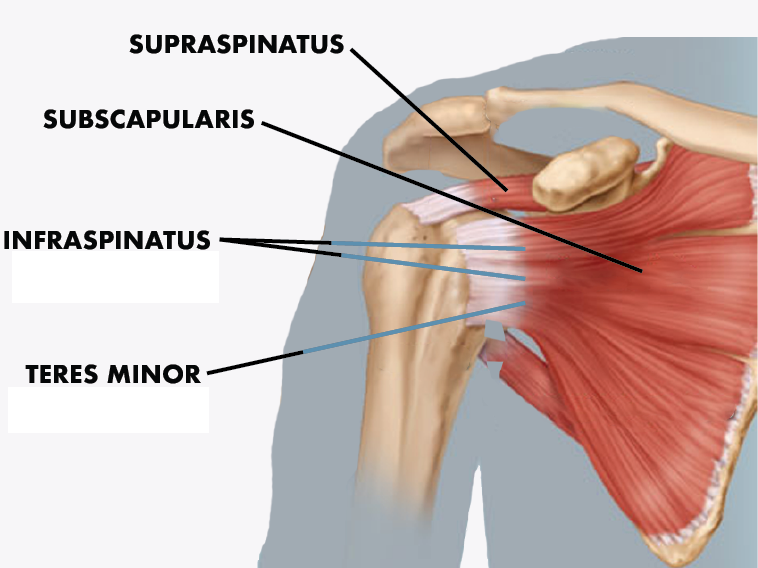
One of, if not the, most commonly injured part of the shoulder is the rotator cuff. The rotator cuff is a designation given to a series of four (4) muscles and tendons that surround the shoulder joint. Those groups include the supraspinatus, infraspinatus, teres minor, and subscapularis.
While each group has its own functional responsibility within the shoulder, the rotator cuff muscles and tendons collectively work in concert to allow the arm to be lifted and rotated. Specifically, the supraspinatus holds the top end (proximal) of the humerus bone into the shoulder socket. It keeps the upper arm stable and allows the arm to be lifted. If you are experiencing problems lifting the arm to shoulder height or above, the supraspinatus muscle may have been damaged. The supraspinatus muscle, along with the infraspinatus muscle, are the two rotator cuff groups that are most often affected due to trauma.
The second of the rotator cuff groups is the infraspinatus. The infraspinatus is what provides joint stabilization and allows for external rotation of the arm at the shoulder. Moving the arm in an outward direction or attempting to reach beyond oneself may be affected with damage to this muscle.
The subscapularis muscle is triangular piece of muscle that conversely provides for internal rotation of the arm and stabilization of the shoulder. And the teres minor is the smallest of the rotator cuff groups and helps to stabilize the humerus when the shoulder moves. These latter two muscles are less often associated with specific traumatic injuries compared to the supraspinatus and infraspinatus areas.
Treatment for rotator cuff injuries varies based upon the severity of the injury. Rotator cuff damage can be categorized as tendonitis, a partial tear, or a full/complete tear. Shoulder tendonitis is the general term describing inflammation of any of the rotator cuff muscles and tendons. This is often the product of overuse and irritation within the shoulder. Immobilization and anti-inflammatory medication are the most common forms of treatment for tendonitis.
A partial tear of the shoulder can occur traumatically or can be the result of wear-and-tear of the shoulder over time. Most partial tears of the rotator cuff muscles can be treated non-operatively with physical therapy and pain medication but may require surgery if the complaints of pain or limitation persistent over time. Full or complete tears of the rotator cuff are mostly commonly associated with acute events, such as fall or trauma to the shoulder. Complete tears will often require surgical management in the form of an arthroscopic or open repair of the muscle and tendons.
B. Labrum Tears
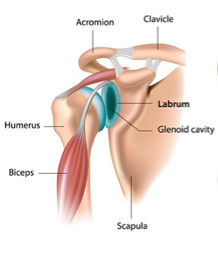
The labrum is an oval piece of thick cartilage that lines the rim of the shoulder socket, known as the glenoid bone. The cartilage serves as a “bumper” between the humeral head (the ball of the upper arm bone) and the glenoid. Stated simply, the humeral head is the ball and the glenoid is the socket. But the socket is not as deep and wide as the ball. The labrum lines this socket and helps keep the humeral head in place. The labrum also has ligaments attached that help hold the entire joint together.
The most common injury that causes damage to the labrum is a traumatic subluxation or dislocation of the shoulder. In these types of injuries, the humeral head is pulled partially or fully out of the socket. During that process, the cartilage of the labrum can become detached from the glenoid. Additionally, the ligaments attached to the labrum can tear.
While a dislocated shoulder can be set back into place, damage done to the labrum due to the initial dislocation will cause instability and will increase the chances that the shoulder dislocates again and again. Weakness and instability, along with a feeling that the shoulder is “slipping out of place,” are the major indicators of a labral shoulder injury.
Surgery to repair the labrum may take multiple forms including:
Bankart repair. A Bankart lesion is a tear that forms in the lower rim of the labrum. This type of tear is the result of ligaments being torn from the front of the socket. Surgery to repair a Bankart lesion involves reattaching the labrum to the glenoid.
SLAP repair. SLAP is an acronym for “superior labrum from anterior to posterior,” meaning that the tear runs front to back in the upper portion of the labrum. The tear occurs at the point where one of the tendons of the biceps muscle inserts on the labrum. Surgery involves using small anchors attached to sutures to reattach the torn portion of the labrum to the bone.
While labral tears can be treated non-operatively with medications, physical therapy, and pain management injections, the cartilage and tearing cannot be “fixed” without surgery to repair the damage. The recovery time from such a procedure will depend if it is done arthroscopically or with a full open incision but is usually in the 3-6 month range.
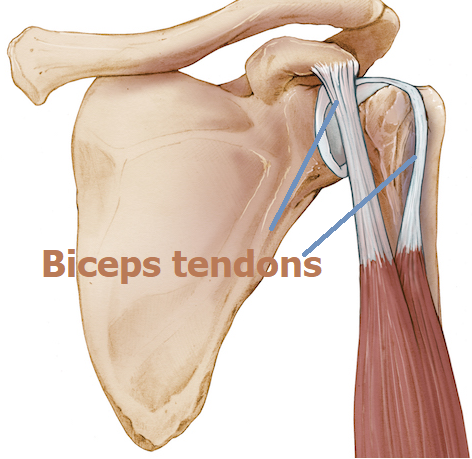
Most people do not associate the biceps with shoulder anatomy; however the biceps include two large tendons that attach the biceps muscle to the bones of the scapula.
When one or both of these tendons are torn, attendant symptoms include an audible snapping or cracking sound, tenderness, sharp pain, bruising and weakness. Additionally, in the event of a tear, the biceps muscle can bunch together and form a large, painful knot on the upper arm known as a “Popeye deformity” given the resemblance to the well-known, post-spinach biceps anatomy of the cartoon character bearing its name.
As with all muscle and ligament tears discussed, treatment options will vary depending on the extend of the injury. Full or near full tears are more likely to require surgery. Incomplete tears may not require surgery depending on the persons age, occupation, and level of activity. The surgery performed for a biceps tendon tear can involve suturing the soft tissues, or may involve use of hardware such as screws. The surgery can also be performed on an open or arthroscopic basis.
CASE STUDY
Our client at Weir Attorneys was a 65-year-old female who sustained a trip-and-fall injury on an uneven sidewalk in Princeton, New Jersey. The slabs of the sidewalk did not meet flush but were rather offset by nearly 1 inch, in violation of American Society for Testing and Materials (ASTM) code, which caused our client to trip and fall. Our client was unable to extend her hand in time and fell directly on her left shoulder – a direct impact injury.
The impact to the client’s left shoulder caused an immediate dislocation of her humeral head from the glenoid and an avulsion fracture of the greater tuberosity. She was taken to the emergency room where her shoulder was set and immobilized. She was discharged from the ER and advised to follow up with an orthopedic surgeon. Her orthopedist prescribed an MRI of the shoulder, which revealed a large full thickness tear of the supraspinatus tendon as well as an avulsion fracture of the greater tuberosity.
Given the client’s active lifestyle and desire to gain back as much functionality in the shoulder as possible, she underwent an arthroscopic procedure to repair the supraspinatus tendon using a horizontal mattress suture and standard knot-tying technique. During the procedure it was also discovered that that client had a degenerative tear of the Labrum and some age-appropriate bone spurring, which likely predated her fall but could have been aggravated by the incident. The bone spurring, which tends to cause further wearing down of muscles and tendons, was shaved back and smoothed over. The labral tear was repaired using sutures. The same-day surgery was performed without complication.
Following her surgery, our client was extremely diligent in pursuing a course of formal physical therapy for approximately six (6) months. Even after discharge from formal therapy, she continued to perform home exercises daily. Fortunately for our client, through the skill of her surgeon and her post-operative rehabilitation efforts, she was able to regain 95-100% of the functionality of her left shoulder.
Our office pursued monetary recovery on behalf of our client for her medical bills and the pain and discomfort she experienced due to her injury. We asserted a claim against the commercial property owner that was responsible for properly maintaining the sidewalk where our client fell and that owner’s insurance company. The case ultimately settled before going to Court for the sum of Two Hundred Fifteen Thousand Dollars ($215,000.00), which included approximately Ten Thousand Dollars ($10,000.00) in medical bills and Two Hundred Five Thousand Dollars ($205,000.00) for our client’s pain and suffering. *
At Weir Attorneys we have extensive experience in prosecuting and defending cases involving a multitude of shoulder injuries that are treated operatively and non-operatively. Taking the time to understand that not all shoulder injuries are alike is the key to properly litigating these types of personal injury matters and maximizing results on behalf of our clients.
* Past performance is no guarantee of future results